Many people begin recovery with determination, only to find themselves relapsing after completing standard treatment programs. Despite their best efforts, the generic nature of many rehab approaches – uniform detox protocols, rigid therapy formats, and limited aftercare – often fails to address the underlying complexities of each individual’s experience.
Personalized addiction care offers a different path. By tailoring treatment to a person’s biology, trauma history, mental health, and daily life, this approach moves beyond diagnosis to focus on the whole individual. The result is a more flexible, targeted form of care designed to support lasting recovery.
Why Standard Opioid Treatment Fails (And How Personalization Helps)
Traditional rehab often takes a blanket approach – the same detox protocols for everyone (regardless of metabolism, co-occurring disorders, withdrawal symptoms, and so on), a rigid approach to treatment, and limited aftercare despite relapse risks being highest post-treatment.
Aside from those, the gaps in generic addiction care include ignoring biological differences and other underlying conditions such as chronic pain, overlooking various psychological and social factors that are possibly at play, disregarding personal beliefs and values of patients (examples range from being forced to participate in faith-based programs to not being allowed to try out alternative therapy options), and so on.
Luckily, personalized care addresses these challenges by providing medication-assisted treatment (MAT) tailored to the individual, therapy approaches aligned with their specific needs, and recovery support services designed to fit their daily life and circumstances.
Personalized care offers MAT through the following: genetic testing to determine what drugs work best for treatment and dosing regimens adjusted based on metabolism rates (via medical tests).
In addition, personalized care provides therapy that’s a perfect fit. Post-traumatic stress disorder (PTSD) – Trauma-informed care. Social anxiety – Small-group settings over large meetings.
Lastly, a personalized opioid addiction treatment program offers recovery that supports one’s lifestyle. This includes flexible scheduling for working professionals and what not.
Personalized Care and Treatment in Action
Want to learn how personalized care and treatment spring into action? Read on.
Precision Medication Management
Standard dosing doesn’t work for everyone. In one case, a patient experienced multiple relapses before a genetic test revealed they were an ultra-rapid metabolizer – meaning the medication left their system too quickly to be effective. With this insight, their doctor adjusted the treatment plan, introducing a new regimen and close monitoring. Tools like pharmacogenetic testing and screening for co-occurring conditions help guide these kinds of personalized decisions, improving outcomes where standard protocols fall short.
Customized Therapy Approaches
Group therapy isn’t always the right fit, especially for individuals with a history of trauma. One patient, for instance, withdrew entirely in a group setting due to unresolved childhood experiences. A personalized approach replaced that with one-on-one sessions and therapies better aligned with their needs – including Cognitive Behavioral Therapy (CBT) to reshape habits, Motivational Interviewing (MI) to support early-stage engagement, and commitment-based methods to help manage chronic pain.
Individualized Aftercare Plans
One patient continued to relapse after rehab because their social circle – intended to support sobriety – included people connected to their former drug use. With guidance from a recovery coach, they began volunteering and gradually built a healthier network of supportive connections.
Additional personalized aftercare options can include peer recovery specialists with lived experience, vocational rehabilitation to support job readiness, and family therapy to help repair and strengthen personal relationships.
All of those are made possible thanks to personalized care for recovering patients eager to go down the path to wellness and achieve a better quality of life.

Designing Your Personalized Recovery Path
Personalized care begins with a collaborative process between the individual and their provider to develop a treatment plan tailored to their unique needs. This approach typically follows several structured steps:
Step 1: Comprehensive Assessment
The process starts with an in-depth assessment covering medical factors (such as genetic testing and withdrawal risk), psychological history (including trauma and mental health diagnoses), and the individual’s social environment and support systems. This provides a clear understanding of the person’s starting point.
Step 2: Customized Treatment Planning
After undergoing the first step, a custom wellness and treatment plan will be laid down. That includes medication based on your genetics and other health factors, therapy, and social environment situation.
Step 3: Ongoing Adaptation
Recovery plans are continually adjusted through regular check-ins. Medication or therapy may be modified as needed, and tools such as wearable sobriety trackers provide real-time data to support more responsive care.
Step 4: Community and Purpose
Having a sense of purpose is linked to more successful recovery outcomes. Personalized care supports this by involving patients in meaningful activities and connecting them with peer groups that reflect their values, identity, and lived experiences.
Recovery on Your Terms
Addiction is not a character flaw – it results from a complex interaction of biological, environmental, and personal factors. Personalized care acknowledges this complexity by creating recovery plans tailored to the individual’s specific circumstances.
No one should be expected to fit into a predefined model of recovery. With the right individualized support, sustained wellness becomes not only achievable but realistic.
There is no single path to wellness. What proves effective for one person may not suit another, which is why individualized support plays a critical role in achieving lasting recovery. When care strategies are adapted to the person’s unique needs, they are better positioned to regain stability, improve well-being, and lead a healthier life.
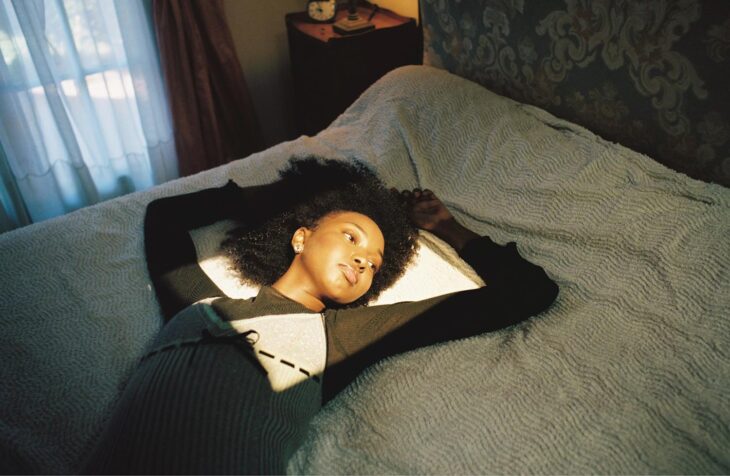
Images from Depressing Holidays by Hoa & Elina Lankry – see full article here.